
Your menstrual cycle is a beautiful, complex dance of hormones — but it doesn’t have to feel complicated to understand. Once you know what’s happening at each stage, it becomes much easier to tune in to your body’s natural rhythms and support yourself through the month. Let’s take a look at the key phases of your cycle and what your hormones are up to behind the scenes.
Day 1–13: Follicular Phase
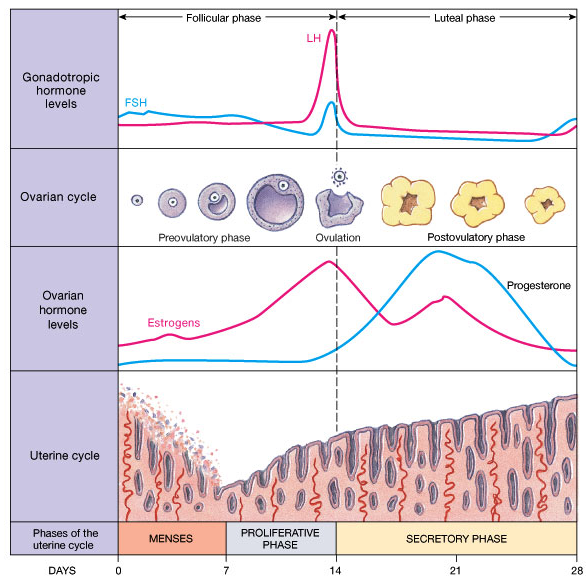
Day 1 of your cycle is marked by the first day of your period — when your hormone levels are at their baseline. This is often why many women feel a sense of relief from PMS symptoms once bleeding begins. During the follicular phase, follicle-stimulating hormone (FSH) and oestrogen work together to build up the uterine lining and mature an egg in preparation for ovulation. Progesterone isn’t in the picture just yet — its role comes later.
Day 14: Mid-Cycle Ovulation
As oestrogen (specifically estradiol) continues to rise and the egg reaches maturity, this triggers a surge in luteinising hormone (LH) — a key event that stimulates ovulation. Ovulation is a very important part of the cycle — no ovulation, no progesterone! After ovulation, both LH and FSH levels drop back down, having completed their role for the month.
Day 15–28: Luteal Phase
After ovulation, you enter the luteal phase — the second half of your cycle. The leftover follicle (now called the corpus luteum) begins producing progesterone, which helps maintain the uterine lining. Oestrogen is still present during this phase, but what’s key is that progesterone now takes centre stage, dominating over estradiol.
End of Cycle
If conception occurs, progesterone and oestrogen levels continue to rise to support the early stages of pregnancy. If pregnancy doesn’t occur, both hormones gradually decline — and this hormonal drop is what triggers your period to begin once again, marking the start of a new cycle.
While we don’t all fit neatly into just four categories, there are some common symptoms that can pop up — either on their own or in various combinations. If any of these sound familiar, it may be worth taking a closer look at your hormonal health:
If you suspect you may have a hormonal imbalance, testing can provide valuable insights and help guide your treatment plan. A great place to start is with some basic blood tests, which you can organise through your GP or your practitioner.
One advantage of testing via your GP is that many of these tests are publicly funded — whereas if your practitioner orders them privately, there may be an out-of-pocket cost. There are also more in-depth testing options available through private labs, such as the DUTCH and EVE hormone tests, which can give a more comprehensive view of your hormone picture. Please Contact Us if you’d like to explore these options further.
Here’s a guide to when and what to test:
👉 Cycle Days 2–3 (Day 1 = first day of your period)
FSH (Follicle Stimulating Hormone)
LH (Luteinising Hormone)
Estradiol
Prolactin
Testosterone
👉 Day 21 or Mid-Luteal Phase
(Keep in mind that your mid-luteal phase may fall later than Day 21 if you have a longer cycle.)
Progesterone
Estradiol
👉 Thyroid Function
TSH (Thyroid Stimulating Hormone)
Free T4 (FT4)
Where possible, I also recommend testing Free T3 (FT3), Reverse T3 (RT3), and thyroid antibodies — although accessing these tests is becoming increasingly challenging in NZ.
👉 Other Key Markers
Iron studies
Liver function
Final thoughts:
Trying to unravel what’s going on with your hormones can feel confusing — and at times, downright frustrating. This is where working with an experienced practitioner can make all the difference. A knowledgeable guide can help you interpret your results and navigate the intricate world of hormonal health with clarity and confidence.
Please place orders before Tuesday 16th December for delivery before Christmas. Orders placed over the holiday period will be sent after Monday 5th January.
Wishing you a Merry Christmas and Happy New Year.
Sign up to get access to announcements, recipes, special deals and more.